What is Uterine Atony?
Uterine atony is a condition that occurs when the uterus does not contract (tighten) properly during or after childbirth. It is a serious complication that can cause life-threatening blood loss.
During pregnancy, the baby is in the womb and receives blood, oxygen, and nutrients from the placenta. Blood vessels and arteries supply blood to the baby through the placenta.
After delivery, the uterus contracts to expel the placenta.
These contractions help to slow down the bleeding by pressing on the blood vessels that connect the uterus to the placenta.
Without pressure on the blood vessels, the blood vessels can leak blood freely and cause postpartum hemorrhage.
This condition is excessive bleeding after giving birth.
This disease can also occur during miscarriage or other uterine surgery. This condition is also a complication of normal delivery or cesarean section.
Symptoms of Uterine Atony
A common symptom of uterine atony is prolonged uterine bleeding. This can cause the sufferer to lose a lot of blood.
Bleeding after delivery is common. However, if you feel like you are bleeding heavily or have to change your pads frequently, you should tell your doctor.
Uterine atony can cause symptoms such as:
- Low blood pressure (hypotension).
- Rapid heartbeat.
- Pale appearance.
- A little pee.
- Dizzy.
- Unconscious.
Causes of Uterine Atony
The basic cause of this condition is that the muscles of the uterus do not contract. After giving birth, the pituitary gland releases the hormone oxytocin.
This hormone stimulates uterine muscle contractions and stops bleeding.
However, when uterine atony occurs, the uterine muscles do not contract adequately in response to oxytocin.
Risk Factors for Uterine Atony
There are several factors that can prevent the uterine muscles from contracting after delivery. Common factors that trigger uterine atony are:
- Prolonged labor.
- Overdistension (excessive stretching) or excessive enlargement of the uterus due to various causes. Among them are multiple pregnancies and polyhydramnios (large amounts of amniotic fluid).
- Rapid labor.
- Use of oxytocin (a hormone used to produce contractions).
- Use of general anesthesia or other drugs during labor.
In addition to the factors above, there are also several factors associated with an increased risk of uterine atony, namely:
- Fetal macrosomia (a fetus that is larger than normal).
- High parity (having many previous births).
- Intra-amniotic infection or chorioamnionitis (infection of the fetal membranes and amniotic fluid).
- Agents that relax the uterus (such as drugs used to relieve pain during labor).
- Over 35 years old.
- Obesity.
- Delivery involving forceps or vacuum assistance
You need to remember, that uterine atony can occur even in those who do not have any risk factors.
Diagnosis of Uterine Atony
Doctors diagnose uterine atony based on the feel and size of your uterus. If you’re having a cesarean section, your doctor will insert a hand into your uterus through a vaginal exam.
Normally the uterus contracts and shrinks soon after the baby is born. If you have uterine atony, the uterus remains large and feels soft.
Sometimes, atony occurs only in the lower part of the uterus. The upper part (fundus) may feel normal.
Although the doctor will feel the soft texture of uterine atony around the uterus, he or she may focus on the lower area if the fundus feels normal.
About three-quarters of postpartum hemorrhages are caused by uterine atony. To confirm this, your doctor may also perform tests to:
- To find out if there is a tear in the cervix, vagina, or uterus.
- Incomplete delivery of the placenta can also cause heavy bleeding.
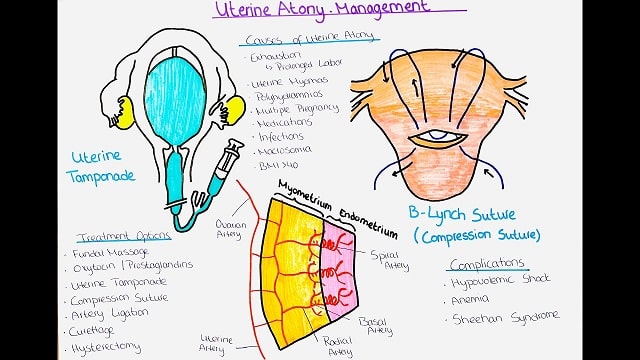
Uterine Atony Treatment
Uterine atony is a condition that requires immediate treatment. Once the bleeding stops, you may need one or more blood transfusions to recover.
Doctors may also give intravenous infusions, oxygen, and other drug treatments if blood pressure is low.
Several medications can help increase uterine contractions and control bleeding, including:
- Oxytocin.
- Methergine.
- Prostaglandin.
- Alkaloid ergot.
- Misoprostol.
For cases of uterine atony accompanied by complications, other treatments may be needed to replace fluids and blood loss. These include:
- Intravenous (IV) fluids.
- Blood transfusion.
- Medicine to restore blood deficiency.
Meanwhile, for very severe uterine atony with complications, the doctor may take the following actions:
- Surgical procedure: to tie off blood vessels.
- Uterine artery embolization: Blocking blood flow to the uterus.
- Hysterectomy: Surgical removal of the uterus when all other treatments fail.
Prevention of Uterine Atony
Not all uterine atony can be prevented. It is important for doctors to know how to treat this condition at all stages of labor.
If you are at high risk of uterine atony, it is best to give birth at a maternal and child health facility or hospital, which has adequate equipment to handle bleeding.
IVs and medications should be readily available. Nurses and anesthesia should be available at all times. It is also important to notify the blood bank of the potential need for blood.
Doctors should also monitor vital signs and the amount of bleeding that occurs after birth to detect bleeding.
Oxytocin given by doctors immediately after delivery can help the uterus contract. In addition, uterine massage immediately after the placenta is born can also reduce the risk of uterine atony.
Taking prenatal vitamins, including iron supplements, can also help prevent anemia and other complications of uterine atony and postpartum hemorrhage.
Complications of Uterine Atony
Some complications of uterine atony are:
- Orthostatic/postural hypotension, which is dizziness due to low blood pressure that usually occurs when someone gets up after sitting or lying down.
- Anemia, low red blood cell count.
- Hypovolemic shock, a serious and potentially life-threatening complication of uterine atony, involves low blood volume due to loss of blood or other fluids.
- Hemorrhagic shock occurs due to blood loss.