Understanding Retinal Detachment
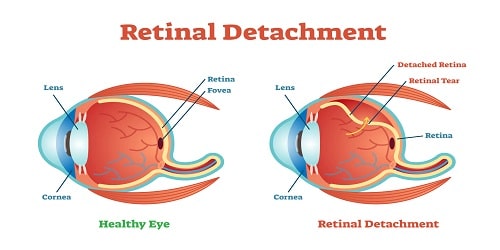
Retinal detachment or retinal detachment is a condition where the retina detaches from its supporting tissue. The retina is a thin layer in the eye that is rich in cells that are sensitive to light. In addition, the retina functions to process the light that is captured and converted into electrical signals which are then transmitted by the optic nerve and interpreted by the brain.
The retina is supported by the layer below it, namely the choroid layer which is rich in blood vessels that provide oxygen and nutrients to the retina. When the retina detaches from this layer, the oxygen supply to the detached part will be disrupted and this affects vision.
Retinal detachment is an emergency condition that can cause permanent vision loss if not treated immediately.
Causes of Retinal Detachment
Detachment of the retina from the layers below is caused by 3 types of mechanisms, each of which has a different cause, namely:
1. Rhegmatogenous
This type of retinal detachment is the most common type. The mechanism underlying retinal detachment is that there is a tear or hole in the retina which allows fluid to pass and collect under the retinal layer, and makes the retina move away from the underlying tissue.
The most common cause of this type is aging. As we age, the vitreous or gel that fills the inside of the eye changes in consistency to become more fluid.
2. Tractional
This type occurs when there is scar tissue on the retina which causes the retina to be pulled away from the back of the eye. This type usually occurs in people with uncontrolled diabetes.
3. Exudative
In this type, fluid builds up under the retina without any tears or holes. This occurs due to fluid from the blood vessels coming out and collecting under the retina. Examples include cases of hypertension, blocked central retinal veins, eye injuries, inflammation of blood vessels (vasculitis), macular degeneration, and tumors.
Risk Factors for Retinal Detachment
There are several risk factors that can increase the risk of retinal detachment, including:
1. Age, retinal detachment often occurs at the age of 50 years and over.
2. History of retinal detachment.
3. Family history of retinal detachment.
4. Have very high myopia or nearsightedness, for example minus 10.
5. History of eye surgery, such as cataract surgery.
6. There is a history of serious eye injury.
7. History of other eye diseases, such as uveitis or inflammation of the middle layer of the eye.
Symptoms
Symptoms of retinal detachment usually occur suddenly. The symptoms of retinal detachment are:
1. Photopsia, seeing flashes of light. These symptoms usually appear early in the disease.
2. There are black spots that always move or float in your vision ( floaters ).
3. The field of view is narrowed, some vision seems to be covered by a gray curtain. These symptoms develop over time and can help determine the location of the detached retina.
Diagnosis of Retinal Detachment
The doctor or vitreoretinal ophthalmologist will ask about symptoms in detail. Then you will perform a physical examination of the eyes, and perform several tests to detect retinal detachment.
1. Physical examination of the eyes
Includes examination of eye vision or visual acuity, examination of the outside of the eye to look for signs of injury to the eye, examination of the pupils, eye pressure in both eyes and examination of the eye’s visual field.
2. Retinal examination
The doctor uses a bright light and special lenses to examine the back of the eye, including the retina. This examination allows the doctor to see any holes in the retina, tears, or detachment of the retinal layers.
3. Ultrasonography (USG) of the eye
This examination is used if bleeding occurs in the eye making it difficult to see the retina.
Retinal Detachment Treatment
Almost all sufferers who experience retinal detachment require surgery to repair tears, and holes, or return the retina to its normal position. Several types of surgery are performed to repair retinal detachment, namely:
1. Photocoagulation or laser surgery
The laser will be directed to the retina through the pupil. The laser will burn around the retinal tear and cause scar tissue that can attach the retina to the layers beneath it.
2. Cryopexy or cryotherapy
Cryopexy uses a special freezing probe to freeze the tissue around the retinal tear. The freezing that occurs helps the retina stick to its underlying layers.
3. Scleral buckle
The scleral buckle procedure places a flexible band on the eyeball to neutralize forces that pull the retina from its normal position.
4. Pneumatic retinopexy
This pneumatic retinopexy procedure uses a certain gas that is injected into the vitreous space inside the eye. The gas will push the retinal tear back into place. This gas will disappear gradually on its own.
The doctor will ask you to maintain the head position for several days. This procedure is often combined with laser surgery or cryopexy.
5. Vitrectomy
The eye doctor will remove the vitreous fluid from the retina. The vitreous will be replaced with air, gas, or oil bubbles. The bubbles push the retina into position so it can heal properly. If an oil bubble is used, the ophthalmologist will remove it several months later.
With air or gas bubbles, sufferers are not allowed to travel by plane, travel to high places or dive in the sea ( scuba diving ). This is because changes in altitude can cause the gas to expand, thereby increasing eye pressure.
After surgery, vision will recover within a few weeks to several months. However, there may be some cases where vision does not recover completely.
In some other cases, retinal detachment cannot be repaired, even with surgical therapy. Usually in cases where there is already extensive scar tissue on the retina. In essence, the more severe the retinal detachment, the less vision will recover.
Prevention
Retinal detachment cannot always be prevented, for example, retinal detachment is caused by the aging process. However, the following efforts can reduce a person’s risk of retinal detachment as follows:
1. Check your eye health regularly, especially if you have risk factors such as diabetes, hypertension or old age.
2. Use eye protection when exercising to reduce the risk of serious eye injury.
3. Immediately visit an eye doctor if floaters, flashes or flashes of light appear, or there are any changes in vision.
4. Routinely check your eyes at least once every year.
5. Examinations should be carried out more frequently if you have diabetes.
6. Routinely control sugar levels and blood pressure, so that the condition of the retinal blood vessels remains healthy.
7. Use eye protection when exercising or when doing activities that risk injuring your eyes.
Complications
Complications can occur if certain treatment procedures are carried out. Some complications that can occur are:
1. The formation of cataracts, or loss of clarity in the lens of the eye.
2. Glaucoma, namely increased pressure in the eye.
3. Infection.
4. Bleeding into the vitreous cavity.
5. Loss of vision.
6. Losing an eye, despite very modern surgical procedures. But this complication is rare.
When Should You See a Doctor?
Retinal detachment is an emergency case in the field of eyes, so if family or relatives have the symptoms above, immediately discuss it with a doctor. Quick treatment of retinal detachment can reduce the risk of permanent blindness complications that can result.