Overview
The pituitary gland or pituitary gland is a small gland located at the base of the brain, often also known as the “queen of the glands”. The pituitary gland is often considered the main endocrine gland, because, together with the hypothalamus, it controls the activity of the entire endocrine system. The pituitary gland is the place of formation or storage of certain hormones.
The hormones secreted by the pituitary gland are: Prolactin (PRL), TSH (thyrotropin), GH (growth hormone), ACTH (adrenocorticotropic hormone), LH (luteinizing hormone), FSH (follicle stimulating hormone)
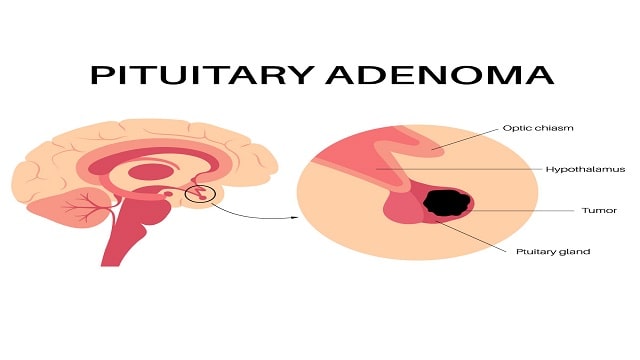
Pituitary tumors are masses of tissue found in the gland. Pituitary adenomas are the most common pituitary tumors. They are benign tumors that spread to other parts of the body, formed by uncontrolled multiplication of one of the 5 types of pituitary cells, able to secrete one or more types of pituitary hormones.
Depending on the size of the tumor, pituitary adenomas are classified:
-microadenomas- tumors smaller than 1 cm in diameter;
– macroadenomas – tumors larger than 1m in size;
Cause
The cause of the development of pituitary adenoma is unknown. At the base of the formation of the tumor mass are alterations in the DNA structure (genetic material that dictates the cell’s mode of operation), so that previously normal cells begin to multiply uncontrollably, without responding to the body’s means of control.
Risk factors that increase a person’s chances of developing a pituitary adenoma include:
Personal or family history of MEN1 syndrome
Personal or family history of Carney syndrome
Isolated familial hypopituitarism
McCune Albright syndrome
symptom
The symptoms can vary from one case to another, depending on the size of the tumor, the secreting or non-secreting form and the type of secreted hormone. The symptoms do not always correlate with the size of the tumor mass. A small, secreting tumor has a noisier feel compared to a larger, non-secreting adenoma.
Symptoms that are determined by the tumor mass syndrome (the tumor, due to its size, compresses the pituitary gland or adjacent structures) may include:
– headache
– visual disturbances (blurred vision, scotoma, loss of vision in one eye)
-epilepsy
– facial nerve paralysis
double vision
– palpebral ptosis (fallen eyelid)
– rhinorrhea (discharge from the nose)
If the adenoma secretes prolactin (40% of cases), the following manifestations may also occur:
– false lactation (secretion from the breasts, in women who do not breastfeed)
– disappearance of menstruation or irregular menstruation
– decrease libido
– vaginal dryness
– low bone density or osteoporosis
The specific symptoms of the thyrotropin-secreting adenoma are:
– enlargement of the thyroid gland
– symptoms of hyperthyroidism
– tremors
– palpitations
– anxiety
– weight loss
– insomnia
The symptoms encountered when the adenoma secretes corticotropin are:
– menstrual disorders
– high blood pressure
– changes in the skin (facial hair, easy bruising of the skin, the appearance of blue lines on the skin)
– rapid increase in blood sugar levels
– thickening of the neck
– obesity with centro-truncular predisposition
– round face, “in the month full”
If the adenoma secretes growth hormones, the following manifestations occur:
– acromegaly (adults)
– gigantism (children)
– hyperglycemia –
excessive sweating
Through compression, the pituitary adenoma can cause pituitary insufficiency, the signs and symptoms being caused by hormonal deficiency:
– slowing down or stopping growth in children
– lack of menstruation
-infertility
– lack of appearance of secondary sexual characters
-loss of facial hair (men)
– lack of pubic hair
– lack of postpartum lactation
– low blood pressure
– intolerance to cold
– weight gain
– thickened skin
-depression
-difficulty concentrating
-excessive fatigue
– low glycemic values
Diagnostic
The endocrinologist will ask the patient for details related to the medical history and symptoms and will perform a complete physical examination. Investigations may include blood tests to measure the values of hormones produced by the pituitary gland and other glands (prolactin, TSH, FT4, IGF-1, growth hormones, corticotrophin or ACTH, human beta-gonadotropin, testosterone, estradiol), hormone levels and blood sugar.
Imaging tests
Nuclear magnetic resonance is the gold standard in the diagnosis of pituitary tumors.
Computed tomography – an important imaging investigation in the management of pituitary adenomas, can bring additional information about the structure of the tumor and its neighboring structures.
Treatment of pituitary adenoma
The treatment of pituitary adenoma involves a multidisciplinary team made up of a neurologist, endocrinologist and ophthalmologist. This may involve monitoring the evolution of the tumor and timing the initiation of treatment, administration of drugs, radiotherapy or surgical excision of the tumor.
Follow-up of the evolution of the pituitary adenoma
Your doctors will recommend the frequency of medical visits and repeat blood tests and imaging investigations. If the pathology is accentuated or the tumor mass changes, one of the therapeutic options will be resorted to.
Drug treatment
It represents an extremely valuable therapeutic alternative, with the aim of:
-inhibits the hormonal secretion of the tumor
-replaces the hormonal deficit caused by the compression caused by the pituitary adenoma
-reduces the tumor to prevent it from compressing the pituitary gland or the structures adjacent to it
Radiotherapy is useful in the following situations:
– when the surgical intervention cannot remove the entire tumor mass
-pituitary adenoma reappears after surgery
– the tumor mass does not decrease after drug treatment
– the tumor mass is located in an area of the brain with increased surgical risk
The surgical treatment is rarely performed by opening the skull, most often using the transsphenoidal approach.