Dyslipidemia
Dyslipidemia refers to unhealthy levels of one or more types of lipids (fats) in the blood. Blood itself contains three main types of lipids, namely:
- High-density lipoprotein (HDL).
- Low-density lipoprotein (LDL).
- Triglycerides.
If you have dyslipidemia, it usually means your LDL or triglyceride levels are too high. It can also mean your HDL levels are too low.
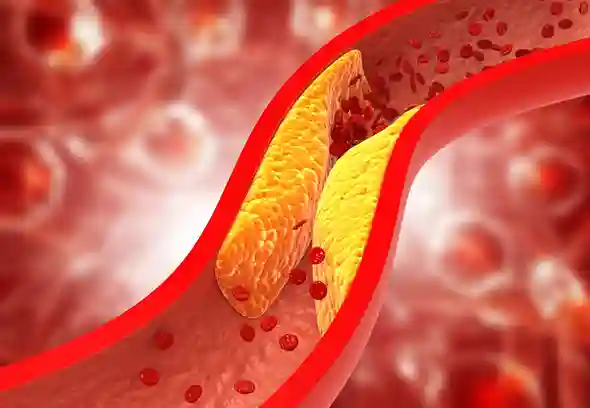
In the medical world, LDL cholesterol is considered the “bad” type of cholesterol. That’s because it can build up and form clots or plaques on artery walls. Too much plaque in the heart’s arteries can lead to a heart attack. Meanwhile, HDL is the “good” cholesterol because it helps remove LDL from the blood.
Finally, triglycerides come from calories you eat but don’t burn right away. Triglycerides are stored in fat cells. They’re released as energy when you need it. If you eat more calories than you burn, you can build up triglycerides.
High LDL and triglyceride levels can put you at risk for heart attack and stroke. Low HDL cholesterol levels are also linked to a higher risk of heart disease.
Symptoms of Dyslipidemia
Most people with dyslipidemia don’t realize they have it, unless the condition is quite severe. A doctor will usually diagnose dyslipidemia during a routine blood test or a test for another condition.
Severe or untreated dyslipidemia can lead to other conditions, including coronary artery disease (CAD) and peripheral artery disease (PAD). Both CAD and PAD can lead to serious health complications, including heart attack and stroke. Common symptoms of these conditions include:
- Leg pain, especially when walking or standing.
- Chest pain.
- Tightness or pressure in the chest and shortness of breath.
- Pain, tightness, and pressure in the neck, jaw, shoulders, and back.
- Indigestion and heartburn.
- Sleep problems and daytime fatigue.
- Dizzy.
- Heart palpitations.
- A cold sweat.
- Vomiting and nausea.
- Swelling in the feet, ankles, legs, abdomen, and blood vessels in the neck.
- Faint.
These symptoms may worsen with activity or stress and improve when a person rests. Talk to your doctor about chest pain, especially if the above symptoms accompany it. Anyone who experiences severe chest pain, dizziness, fainting, or trouble breathing should seek emergency care.
Causes of Dyslipidemia
Dyslipidemia is divided into primary and secondary types. Primary dyslipidemia is passed down from generation to generation. While secondary dyslipidemia is an acquired condition. That condition means it develops from another cause, such as obesity or diabetes.
You may hear the term hyperlipidemia used interchangeably with dyslipidemia. However, this is not entirely accurate. Hyperlipidemia refers to high levels of LDL or triglycerides. Dyslipidemia can refer to levels that are higher or lower than the normal range for these blood fats.
Among the specific types of primary dyslipidemia are:
- Familial Combined Hyperlipidemia. This is the most common cause of high LDL cholesterol and high triglycerides. If you have familial combined hyperlipidemia, you may develop these problems in your teens or 20s. You are also at higher risk for early coronary artery disease, which can lead to heart attacks.
- Familial Hypercholesterolemia and Polygenic Hypercholesterolemia. Both are characterized by high total cholesterol. You can calculate total cholesterol by adding your LDL and HDL levels, along with half your triglyceride level. A total cholesterol level below 200 milligrams per deciliter (mg/dL) is best.
- Familial Hyperbetalipoproteinemia. This condition means you have high levels of apolipoprotein B, a protein that is part of LDL cholesterol. Hyperlipoproteinemia is a condition that can be primary or secondary. If you have this condition, your body has difficulty breaking down LDL cholesterol or triglycerides.
Dyslipidemia Risk Factors
Several factors are known to increase a person’s chances of developing dyslipidemia and related conditions. These risk factors include:
- Obesity.
- A sedentary lifestyle.
- Lack of regular exercise or physical activity.
- Alcohol use.
- Use of tobacco cigarettes.
- Use of illegal drugs.
- Sexually transmitted infections.
- Type 2 diabetes.
- Hypothyroidism.
- Chronic kidney or liver conditions.
- Indigestion.
- Older age.
- A diet high in saturated fat and trans fat.
- Having a parent or grandparent with dyslipidemia.
- Being female, as women tend to experience higher LDL levels after menopause.
Dyslipidemia Diagnosis
A simple blood test to check your LDL, HDL, and triglycerides will reveal whether your levels are high, low, or within the healthy range. These numbers can change from year to year, so it’s a good idea to have your blood tested regularly, such as once a year. However, if you take medication for dyslipidemia, your doctor may want to test your blood more often.
Dyslipidemia Complications
Untreated dyslipidemia can cause plaque to build up in the body’s blood vessels (atherosclerosis). This can lead to complications that include:
- Heart attack.
- Stroke.
- Coronary heart disease.
- Carotid artery disease.
- Sudden heart attack.
- Peripheral artery disease.
- Microvascular disease.
Dyslipidemia Treatment
The most common medications used to treat dyslipidemia are statins. Statins help lower LDL levels by interfering with the liver’s production of cholesterol. There are several types of statins. They all work slightly differently, with some being stronger than others.
Your doctor may also prescribe other cholesterol medications. They can be taken in addition to a statin or instead of a statin. There are many pros and cons to consider when choosing between cholesterol-controlling medications. These non-statin medications include:
- Ezetimibe (Zetia).
- Fibrat, fenofibrate (Fenoglide) supplements.
- PCSK9 inhibitors.
Lifestyle changes can help control cholesterol and triglyceride levels. The first step is to change your diet. Changes should include consuming less saturated fat, refined sugar, and alcohol. Adding more fruits, vegetables, lean proteins, and whole grains to your daily diet can also help.
Daily exercise and weight loss can also help improve your cholesterol profile.
Prevention of Dyslipidemia
Try to maintain a healthy weight by following a heart-healthy diet and exercising regularly. You should also quit smoking if you smoke.
If you are concerned about dyslipidemia, talk to your doctor about how you can prevent it. Also, if you have a family history of high cholesterol, be proactive about living a healthy lifestyle before your cholesterol starts to move to unhealthy levels.
When to See a Doctor?
Continuous dyslipidemia can cause various complications, the most dangerous of course in heart disease and stroke complications. For that, make sure to always apply a healthy lifestyle and take medication recommended by your doctor.