Acute Respiratory Distress Syndrome
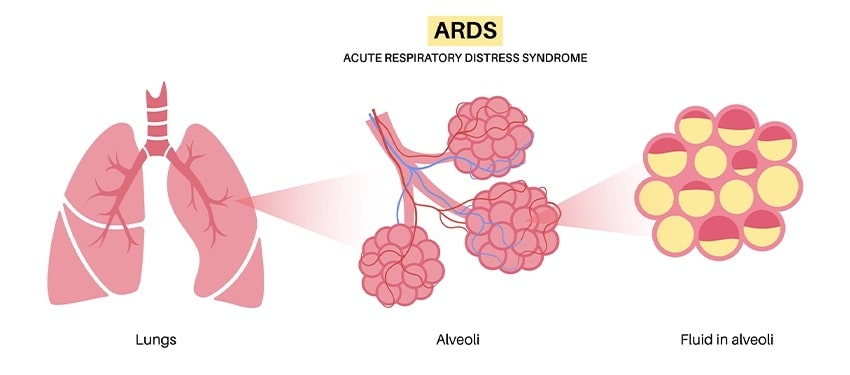
Acute respiratory distress syndrome (ARDS) occurs when fluid builds up in the tiny, elastic air sacs (alveoli) in the lungs. The fluid prevents the lungs from filling with enough air, meaning less oxygen reaches the bloodstream. This deprives organs of the oxygen they need to function.
According to various studies, some people infected with COVID-19 can experience ARDS in the development of their disease. This condition usually occurs in people who are already critically ill or who have significant injuries. Severe shortness of breath as the main symptom of ARDS also usually develops within hours to days after the injury or infection that triggered it.
Many people who develop ARDS do not survive. The risk of death increases with age and the severity of the disease. Of those who survive ARDS, some make a full recovery while others are left with permanent damage to their lungs.
Symptoms of Acute Respiratory Distress Syndrome
Signs and symptoms of ARDS can vary in intensity, depending on the cause and severity, as well as the presence of underlying heart or lung disease. Symptoms include:
- Severe shortness of breath.
- Difficult and unusually rapid breathing.
- Low blood pressure.
- Extreme confusion and exhaustion.
Risk Factors for Acute Respiratory Distress Syndrome
Most people who develop this condition have already been hospitalized for another condition, and many are already critically ill. A person is at particular risk if they have a widespread infection in their bloodstream (sepsis).
People with a history of chronic alcoholism are at higher risk of developing ARDS. They are also more likely to die from the condition.
Causes of Acute Respiratory Distress Syndrome
The mechanical cause of this condition is fluid leaking from the smallest blood vessels in the lungs into the tiny air sacs where blood is oxygenated. Normally, a protective membrane keeps this fluid inside the vessels. Severe illness or injury can cause damage to the membrane, resulting in fluid leakage.
Meanwhile, the underlying causes of ARDS include:
- Sepsis. The most common cause of ARDS is sepsis, a serious and widespread bloodstream infection.
- Inhaling Harmful Substances. Inhaling high concentrations of fumes or chemicals can cause ARDS, as can inhaling (aspiration) of vomit or a near-drowning episode.
- Severe Pneumonia. Severe cases of pneumonia usually affect all five lobes of the lungs.
- Injury. An accident, such as a fall or car crash, can directly damage the lungs or the part of the brain that controls breathing.
- COVID-19. People who have severe COVID-19 can develop ARDS.
Meanwhile, there are other causes such as pancreatitis (inflammation of the pancreas), massive blood transfusion, and burns.
Diagnosis of Acute Respiratory Distress Syndrome
There is no specific test to identify ARDS. Diagnosis is based on a physical exam, chest X-ray, and oxygen levels. It is also important to rule out other diseases and conditions, such as certain heart problems that can produce similar symptoms.
1. Imaging
Imaging tests include, among others:
- Chest X-ray. A chest X-ray can reveal which parts of the lungs and how much of the lungs have fluid in them and whether the heart is enlarged.
- Computerized Tomography (CT). A CT scan combines X-ray images taken from many different directions into a cross-sectional view of internal organs. A CT scan can provide detailed information about the structures inside the heart and lungs.
2. Laboratory tests
A blood test using blood from an artery in the wrist can measure oxygen levels. Other types of blood tests can check for signs of infection or anemia. If the doctor suspects that the patient has a lung infection, secretions from the airways can be tested to determine the cause of the infection.
Testing through laboratory tests can be:
- Culture or examination of sputum samples, to identify the bacteria or microorganisms causing the infection.
- Biopsy or taking a sample of lung tissue. This test is to eliminate the possibility of symptoms that occur due to lung diseases other than ARDS.
3. Heart Test
Because the signs and symptoms of ARDS are similar to certain heart problems, your doctor may recommend heart tests such as:
- Electrocardiogram. This painless test tracks the electrical activity in the heart. It involves attaching several wired sensors to the body.
- Echocardiogram. A sonogram of the heart, this test can reveal problems with the structure and function of the heart.
Treatment of Acute Respiratory Distress Syndrome
The first goal in treating ARDS is to increase the oxygen levels in the blood. Without oxygen, organs cannot function properly.
1. Oxygen
To get more oxygen into the bloodstream, your doctor will likely use:
- Additional oxygen. For milder symptoms or as a temporary measure, oxygen can be given through a mask that fits over the nose and mouth.
- Mechanical ventilation. Most people with ARDS will need a machine to help them breathe. A mechanical ventilator pushes air into the lungs and forces some of the fluid out of the air sacs.
- Fluids. Carefully managing the amount of intravenous fluids is essential. Too much fluid can increase fluid buildup in the lungs. Too little fluid can overwhelm the heart and other organs and cause shock.
2. Medicines
People with ARDS are usually given medications to:
- Prevent and treat infections;
- Relieves pain and discomfort;
- Prevent blood clots in the legs and lungs;
- Minimizes gastric reflux;
- Keep them calm.
3. Minimize complications
Steps to minimize ARDS complications usually include:
- Sedation to manage pain.
- Breathing tests to determine when it is safe to remove the tube and ventilator.
- Using blood thinners to prevent clotting.
- Minimizes fluid buildup in the lungs.
- Reduces the possibility of stress ulcers in the stomach.
- Be physically active and undergo physical therapy to prevent muscle weakness.
Prevention of Acute Respiratory Distress Syndrome
There is no specific prevention for ARDS, but by knowing the symptoms and signs, doctors can treat it as soon as possible to prevent complications.
In addition, there are several steps that can help protect the lungs, such as:
- If you smoke, seek help to quit, and avoid secondhand smoke whenever possible.
- Getting vaccinated, such as a yearly flu (influenza) shot, and a pneumonia vaccine every five years, can reduce your risk of lung infections.
- Stop drinking alcohol.
- Living a clean and healthy lifestyle.
- Be careful when driving and always wear a seat belt or helmet.
Complications of Acute Respiratory Distress Syndrome
If someone has ARDS, they may develop other medical problems while they are in the hospital. The most common problems are:
- Blood Clots. Being hospitalized while on a ventilator can increase the risk of blood clots, especially in the deep veins of the legs. If a clot forms in the legs, part of it can break off and travel to one or both lungs (pulmonary embolism) where it blocks blood flow.
- Collapsed Lung or Pneumothorax. In most cases of ARDS, a breathing machine called a ventilator is used to increase oxygen in the body and force fluid out of the lungs. However, the pressure and volume of air from the ventilator can force gas through a small hole in the outermost part of the lung, causing the lung to collapse.
- Infection. Because the ventilator is attached directly to a tube that goes down your throat, it makes it easier for germs to infect and further injure your lungs.
- Pulmonary Scarring or Fibrosis. Scarring and thickening of the tissue between the air sacs can occur within a few weeks of the onset of ARDS. This stiffens the lungs, making it more difficult for oxygen to flow from the air sacs to the bloodstream.
Thanks to better treatments, more people are surviving ARDS. However, many survivors end up with potentially serious and sometimes long-lasting effects.
Some of the effects include:
- Breathing Problems. Many people with ARDS recover most of their lung function within a few months to two years, but others may have breathing problems for the rest of their lives. Even healthy people commonly experience shortness of breath and fatigue and may need supplemental oxygen at home for several months.
- Depression. Most ARDS survivors also report experiencing periods of depression.
- Memory and Cognitive Problems. Sedatives and low blood oxygen levels can cause memory loss and cognitive problems after ARDS. In some cases, the effects may lessen over time, but in others, the damage may be permanent.
- Fatigue and Muscle Weakness. Being in the hospital and on a ventilator can cause muscle weakness. A person may also feel very tired after treatment.