Achalasia
Achalasia is classified as a rare disease that can be inherited. Achalasia itself refers to a condition where the esophagus loses its ability to push food from the mouth to the stomach.
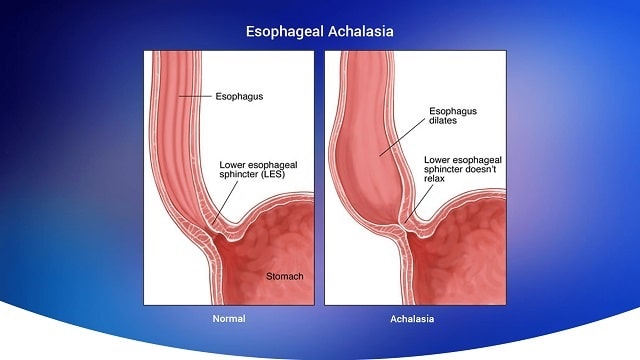
Normally, the Lower Esophageal Sphincter (LES) relaxes, allowing food to enter the stomach. In people with achalasia, the LES does not relax properly, causing food to build up in the lower esophagus or back up into the mouth.
The LES is a ring of muscle located at the bottom of the esophagus. The LES opens and closes on its own to prevent stomach acid from rising into the esophagus.
Achalasia Symptoms
Not all sufferers experience symptoms of achalasia. Most of them have difficulty swallowing food or drink. In addition, symptoms that appear include:
- Food comes back into the mouth, like I want to vomit.
- Coughing when swallowing due to choking.
- Increased production of stomach acid .
- Pain in the chest area.
- Having recurrent chest infections.
- Vomiting saliva due to increased production of stomach acid.
- Weight loss is slow, but it is significant.
These symptoms can be experienced by anyone and can occur at any time. If these symptoms are left untreated, the risk of esophageal cancer increases.
Therefore, immediately take the right treatment steps when you find the symptoms.
Achalasia Risk Factors
The main cause of achalasia is nerve damage in the esophagus so that the muscles cannot work properly. In addition to nerve damage, achalasia can also occur due to the following risk factors:
- Suffered a spinal injury.
- Undergoing endoscopic sclerotherapy.
- Having a viral infection.
- Have an autoimmune disease.
- Have a family history.
- Weak immune system in the nerve cells of the esophagus.
- Aged 40-60 years.
- Suffering from Down syndrome.
Types of Achalasia
The way the muscles in the esophagus don’t work in people with achalasia varies. In most cases, the lower esophageal sphincter that controls the passage between the esophagus and stomach is unable to relax at the right time.
Based on other problems that occur together, doctors identify three types of achalasia, namely:
- Achalasia type 1 (classic achalasia) . In this type, the esophageal muscles barely contract, so food moves down only due to gravity.
- Achalasia type 2. Pressure builds up in the esophagus, causing it to become compressed. This is arguably the most common type of achalasia and often causes more severe symptoms than type 1.
- Achalasia type 3 (spastic achalasia). This type of achalasia has abnormal contractions at the bottom of the esophagus where it meets the stomach. This is the most severe type of achalasia. This is because the contractions can cause chest pain that can wake a person from sleep and the symptoms are similar to a heart attack.
Causes of Achalasia
The exact cause of achalasia is not fully understood. However, researchers suspect that the condition is caused by damage to the nerves in the esophagus, causing them to stop working properly. This causes the muscles and muscle rings in the throat to stop working.
In addition, some other experts suspect that achalasia is related to a viral infection. Achalasia is also associated with autoimmune conditions, where the immune system attacks healthy cells, tissues, and organs.
Meanwhile, in rare cases, achalasia can be inherited in families.
Achalasia Diagnosis
The diagnosis process is carried out by a specialist doctor based on the results of the interview and complaints experienced by the sufferer. Then, the doctor continues the diagnosis process by conducting a physical examination and other supporting tests.
Here are some supporting examinations that you need to do:
- Manometry, which involves inserting a small plastic tube through the mouth or nose into the esophagus to measure muscle pressure along the airway.
- Esophagography, which is done by drinking a white liquid containing barium. The liquid will be clearly visible on X-ray. Its purpose is to see how long it takes to enter the stomach.
- Endoscopy, which is performed using fiber optics and a camera to directly view the lining of the patient’s esophagus, muscular ring, and stomach.
Achalasia Treatment
Treatment for achalasia aims to open the LES muscle, allowing food and drink to enter the stomach. Here are some common treatment procedures:
1. Medicines
Taking medication from a doctor can help relax the muscles in the esophagus, making the swallowing process easier and less painful.
This procedure does not necessarily work for everyone, and the effects are short-lived. The use of medication usually serves to relieve symptoms, while waiting for other treatments.
2. Muscle stretching
Before the procedure, the patient is first given general anesthesia. Then, the doctor inserts a balloon-like object, which is then pumped up to help stretch the throat muscle ring.
The goal is to increase the elasticity of the muscles when swallowing. This procedure carries a small risk of tearing the esophagus, which would require emergency surgery.
3. Botox injection
Botox fluid is inserted into the esophagus using an endoscope, and injected into the muscle ring. The goal is to relax the throat muscles so that swallowing is not painful.
Although effective, the procedure must be repeated over several months to years. This method is an alternative for people who cannot undergo other treatments.
4. Operation
The surgical procedure involves cutting the ring muscle, allowing food to pass into the stomach. The results are permanent, and make it easier for sufferers to swallow without pain.
When these methods do not work, some people may need surgery to remove part of their esophagus.
5. Peroral Endoscopic Myotomy (POEM)
POEM is a procedure performed using a tool called an endoscope. The tool is equipped with a camera and flashlight on the end to obtain images of the esophagus, stomach, small intestine, and large intestine.
This procedure aims to reduce muscle stiffness so that food and drink can easily flow into the stomach.
In general, peroral endoscopic myotomy is performed with the following steps:
- The ENT specialist will insert an endoscope tube through the mouth to the esophagus. The doctor controls the direction of this tool by looking at the images taken by the camera at the end of the endoscope.
- In addition to the light and small camera, the endoscope also has a special small knife on the end. While the tool is in the esophagus, the small knife will cut and relax the stiff esophageal muscles that trigger swallowing problems.
- The small knife can cut and relax the muscles on the sides of the esophagus, the lower esophageal valve, and the upper part of the stomach.
- Once completed, a clamp will be inserted into the wall of the esophagus to keep the incision closed.
- Next, the endoscope tube will be removed through the patient’s mouth.
6. Pneumatic dilation
This treatment is performed using a balloon-like device, which is inserted endoscopically into the middle of the esophageal sphincter and inflated to enlarge the opening. This outpatient procedure may need to be repeated if the esophageal sphincter does not stay open.
Nearly one-third of people treated with balloon dilation require repeat treatment. At least within five years. In addition, the procedure requires sedation.
As with other treatment procedures, a number of steps to overcome achalasia can also trigger complications. Some conditions that become complications of achalasia treatment, such as holes in the esophagus, bloating, chronic digestive disorders, and the return of achalasia symptoms.
Achalasia Prevention
If caused by genetic factors, there are no preventive measures that can be taken. However, you can do an early examination, so that a number of symptoms that appear can be treated with the right steps.
Here are some steps to prevent achalasia:
- Quit smoking.
- Increase your consumption of water while eating.
- Chew food until completely smooth before swallowing.
- Do not consume foods that can trigger increased stomach acid, such as spicy, sour foods, and foods and drinks containing caffeine.
- Eat small portions but often.
- Do not consume food close to bedtime.
- Position your head higher when sleeping.
Achalasia Complications
Generally, complications of achalasia arise due to a number of symptoms experienced not being addressed with proper treatment steps. Complications occur gradually, starting from increasing difficulty in swallowing food and drink, to weight loss due to malnutrition.
Here are other complications:
- Esophageal or throat cancer.
- Stomach acid rises into the esophagus.
- Pneumonia which causes food to enter the lungs.
- Esophageal perforation is the tearing of the esophageal wall.