Hepatic Encephalopathy Definition
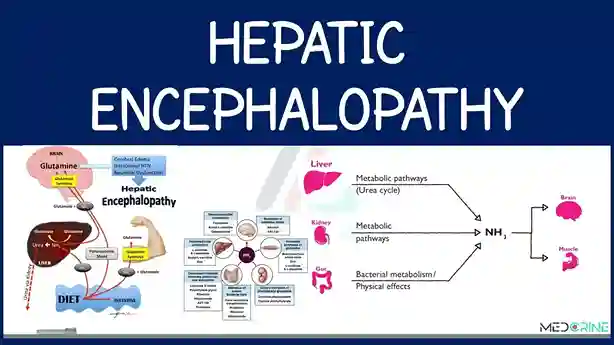
Hepatic encephalopathy (HE) is a common and serious complication of chronic liver disease and acute liver failure. The affected liver struggles to filter toxins (substances produced from the breakdown of food, alcohol, drugs, and even muscle) from the bloodstream. These toxins build up in the body and travel to the brain. The toxicity affects brain function and causes cognitive impairment.
HE manifests as a wide spectrum of neuropsychiatric abnormalities, from subclinical changes (mild cognitive impairment) to disorientation, confusion, and coma.
HE can be classified according to the underlying disease, severity of manifestation, duration of disease, and presence of triggers. There are three types of hepatic encephalopathy based on the underlying disease:
- Type A, caused by acute liver failure (without underlying chronic liver disease).
- Type B, occurs in some people who have a shunt connecting two veins in the liver, without underlying chronic liver disease.
- Type C, results from chronic liver disease and scarring (cirrhosis).
Symptoms of Hepatic Encephalopathy
The main symptoms of hepatic encephalopathy are:
- Anxious or irritable.
- Confused and senile.
- Sleepy.
- Mood changes.
- Weak, lethargic and without energy.
- Having problems with coordination or balance.
- Reduced alertness.
- Sleep problems.
- Slurred speech.
Jaundice may also appear as another symptom of encephalopathy. Meanwhile, people with this condition may also have symptoms of liver disease including fluid in the abdomen and swollen legs.
Causes of Hepatic Encephalopathy
Disorders that damage the liver and cause liver failure can result in hepatic encephalopathy. Some of these disorders include viral hepatitis (such as hepatitis B and hepatitis C), severe infections, autoimmune diseases, cancer, and Reye’s syndrome.
Encephalopathy can also be caused by the use of drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and excessive alcohol consumption. People with liver cirrhosis can also develop encephalopathy from the use of analgesics and sedatives.
Risk Factors for Hepatic Encephalopathy
Certain factors may increase the risk of hepatic encephalopathy, including:
- Dehydration.
- Eating too much protein.
- Bleeding in the digestive tract, such as in the intestines, stomach, or esophagus.
- Infection.
- Kidney disorders.
- Lack of oxygen.
- Experiencing electrolyte imbalance.
- Taking certain medications, especially alcohol, some sedatives, pain relievers (analgesics), or diuretics.
Diagnosis of Hepatic Encephalopathy
Basically, there is no examination that can be used as a gold standard in diagnosing hepatic encephalopathy. In hepatic encephalopathy, a complete and detailed medical interview (anamnesis) and physical examination are required.
This is because there are many diseases that can be a differential diagnosis of hepatic encephalopathy, including vascular disorders, metabolic disorders, intracranial disorders, and neuropsychiatric disorders.
In addition, clinical symptoms found in hepatic encephalopathy are not specific to this disease. In anamnesis, it is necessary to know whether there is a history or clinical symptoms of liver disorders. In addition, it is also necessary to know other factors that trigger hepatic encephalopathy.
If it is deemed necessary to undergo further examination, the doctor will usually recommend a series of tests, including:
- A complete blood test aims to check for potential underlying causes, such as anemia, vitamin deficiency, liver function, sugar levels, and infection.
- X-ray.
- CT and MRI scans.
Your doctor may also perform a mental status test to check for subtle changes that occur in the early stages of hepatic encephalopathy. An electroencephalogram (EEG) may also be performed to detect abnormalities in brain activity. However, these tests cannot help distinguish hepatic encephalopathy from other possible causes.
Hepatic encephalopathy may be more difficult to recognize in older people, as early symptoms (such as disturbed sleep patterns and mild confusion) may be attributed to dementia or mistakenly labeled as delirium.
Hepatic Encephalopathy Treatment and Side Effects
The general treatment is to improve tissue oxygenation. Meanwhile, specific treatment is to address the triggering factors for hepatic coma. For example, protein intake is reduced or temporarily stopped, then gradually increased. However, protein intake restriction is still controversial in the treatment of HE.
The protein source given for hepatic encephalopathy is branched-chain amino acids in the hope that the real and fake neurotransmitters will be balanced. With this, ammonia metabolism in muscles can increase. Giving lactulose at a dose of 10-30 milliliters, 3 times/day is also carried out in the hope that ammonia absorption will be hampered by the acidic pH in the intestine. Apart from that, special medicine is also given for intestinal sterilization.
Complications of Hepatic Encephalopathy
Complications of hepatic encephalopathy include:
- Cerebral edema.
- Kidney failure.
- Acid-base disorders.
- Hypoxia.
- Disorders of hemostasis and bleeding function.
- Electrolyte imbalance (hypocalcemia) and metabolic disorders (hypoglycemia).
- Susceptibility to infection.
- Circulatory disorders.
Prevention of Hepatic Encephalopathy
Encephalopathy can be avoided by adopting a healthy and balanced diet, stopping drinking alcohol, exercising regularly, and undergoing regular health checks.