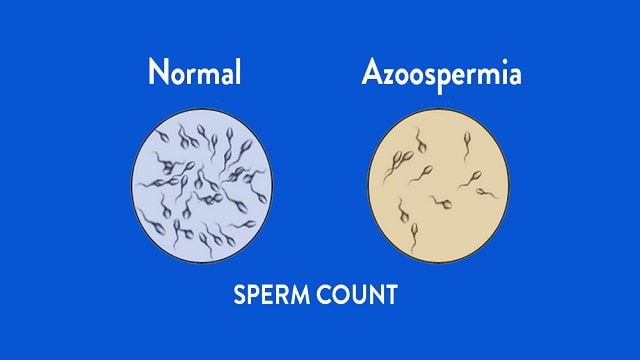
Azoospermia
Azoospermia is a condition where a man’s semen does not contain sperm. This condition is experienced by 1 percent of men worldwide and causes infertility. As many as 10 to 15 percent of infertile men are detected with azoospermia.
The two main types are:
- Obstructive
The obstructive type is caused by a blockage or break in the epididymis, vas deferens, or elsewhere along the reproductive tract. This condition prevents the release of sperm, resulting in no detectable amount in the semen.
-
- Non-obstructive
Non-obstructive type is triggered by poor sperm quality due to defects in the structure or function of the testicles. This condition is usually caused by certain diseases.
Symptoms of Azoospermia
Associated symptoms include:
- Decreased sexual desire.
- Erectile dysfunction.
- Lumps, swelling, or discomfort around the testicles.
- Decreased hair production in the face and body areas.
Causes of Azoospermia
The causes of the disease are classified according to its type:
- Obstructive Azoospermia
Common causes are problems with:
- Epididymis, which is a coiled tube at the back of the testicles.
- Vas deferens, which is the tube that transports sperm from the epididymis.
- The ejaculatory duct, which is the tube through which sperm exits the urethra and mixes with the fluid that forms semen.
Other causes include:
Epididymal obstruction
Several conditions can cause blockages in the epididymis, such as infection, inflammation, and trauma or injury to the scrotum. Another, cystic fibrosis, is a rare genetic disorder that causes blockages or abnormal development. The disorder causes thickening of secretions and leads to a buildup of sperm.
Surgery on the vas deferens
The procedure is called a vasectomy. It involves cutting or clamping the vas deferens to stop the flow of sperm. However, there are other conditions that can have the same effect:
- Trauma or injury. For example, hernia repairs and procedures to address blockages and connections.
- Blockage of the ejaculatory duct. This condition can be caused by infection, trauma, and previous surgical procedures.
- Non-obstructive Azoospermia
Some causes of non-obstructive types include:
Genetics
Genetic disorders and mutations from parents can cause azoospermia problems which can lead to infertility.
Y chromosome deletion
The Y chromosome contains many genes important for sperm. Deletions of the chromosome cause 10 percent of cases of azoospermia. In fact, any male child born to a father with a Y chromosome deletion will inherit the defect.
Karyotype abnormalities
This disorder causes an increase in the X chromosome that results in Klinefelter syndrome. This disorder causes decreased testicular function, sperm count, and testosterone levels in the body.
Radiation and toxins
Exposure to certain substances, such as heavy metals, chemotherapy, pesticides, and radiotherapy increases the risk of azoospermia.
Drugs
One example is testosterone. Excessive consumption will not help improve male reproductive function, but instead increase the risk of azoospermia.
Varicocele
Varicocele is a swelling of the veins in the scrotum. This disorder can reduce sperm production and quality.
Risk Factors for Azoospermia
Some triggering factors that can reduce sperm quality include:
- Thyroid disorders.
- Hyperprolactinemia, which is an increase in the hormone prolactin.
- Genetic disorders.
- Infection.
- Sperm duct abnormalities.
Azoospermia Diagnosis
First of all, the doctor will help detect the history of health problems by asking about the problem. The medical team will ask questions about:
- Success or failure of having children in the past.
- Diseases experienced during childhood.
- Injury or surgery to the pelvic area.
- Urinary or reproductive tract infections.
- History of sexually transmitted infections.
- Exposure to radiation or chemotherapy.
- Current and previous medications taken.
- History of alcohol and drug abuse.
- Family history of birth defects, learning disabilities, reproductive failure or cystic fibrosis.
Next, the doctor will perform a physical examination, such as:
- Checking body shape and reproductive organs.
- Checking for the presence of the vas deferens.
- Check for tenderness or swelling of the epididymis.
- Checking the size of the testicles.
- Checking for blockage of the ejaculatory ducts.
Meanwhile, supporting examinations that will be carried out include:
- Measurement of testosterone and follicle-stimulating hormone levels.
- Genetic testing.
- X-ray or ultrasound (USG) of the reproductive organs to see if there are any problems with their shape and size.
- Brain imaging tests to identify disorders of the hypothalamus or pituitary gland.
- Biopsy or taking a sample of testicular tissue.
Azoospermia Treatment
Treatment steps will depend on the type of disease.
- Obstructive
Disorders can be treated by connecting or reconstructing the sperm tubes or ducts through surgical procedures. Hormonal treatment and medication can also help. This step is taken if the main cause is a decrease in hormone production in the body.
- Non-obstructive
In this type, sufferers may not respond to treatment. If they still want to have children, they can go through in vitro fertilization or intracytoplasmic sperm injection. The procedure is done by extracting sperm from the testicles using a small needle.
Meanwhile, home care steps that can support successful treatment include:
- Eat nutrient-dense foods to boost sperm production.
- Exercise regularly to help increase testosterone levels.
- Yoga or meditation to reduce stress levels in the body. Cortisol (stress hormone) can have an impact on decreasing testosterone production.
Azoospermia Complications
The main complication in sufferers is not being able to have children. This condition can lead to prolonged stress or depression. Meanwhile, complications in the form of bleeding can occur due to medical procedures performed to treat azoospermia.
Azoospermia Prevention
Sufferers can take several steps to improve sperm quality:
- Limiting heavy activity or exercise. Because these activities can harm the testicles and reproductive tract.
- Limit radiation exposure.
- Avoid activities that can expose the testicles to high temperatures, such as saunas or steam baths.